Introduction to Gastro- and Colonoscopies
Gastroscopy is a procedure to observe the esophagus, stomach, and duodenum, inserting a thin tube (approximately 1 cm and 5 mm in diameter for oral and nasal administration, respectively) with a high performance camera mounted at the tip through the mouth or nose.
It facilitates the accurate diagnosis of gastric cancer that develops in more than 100,000 Japanese people annually (the highest prevalence among all cancers) and esophageal cancer, in addition to gastric ulcer, gastritis, and reflux esophagitis, involving stomachache, heaviness in the stomach, heartburn, or other symptoms.
By confirming the presence/absence of atrophic gastritis frequently leading to the development of gastric cancer, it also clarifies the risk of cancer.
Nasogastoscopy, which is a procedure indispensable to diagnose gastritis and gastric ulcer, is also currently starting to play a central role in gastric cancer screening.
Blood testing generally conducted as part of health examinations for company employees is related to gastric cancer only indirectly. Tumor marker (CEA, CA 19-9) values are inappropriate for the prevention and early identification of cancer, as they become abnormal only after cancer has considerably progressed. Barium X-ray tests based on ‘shadow-reading’ are also limited in terms of accuracy and the detection of small or flat lesions.
In contrast, gastroscopy as a method to ‘directly observe the gastric mucosa’ can detect even very small lesions while facilitating accurate diagnosis, as it is also usable for histopathologal examination (biopsy). As a recent trend, suspected gastric disorders are examined using it.

LaLaport Yokohama Clinic performs ‘transnasal gastroscope insertion’ for your comfort
○Inserting an ultra-thin gastroscope from the nose
We use an ultra-thin gastroscope (Olympus GIF-XP260N) with a diameter of 5.0 mm (the thinnest in Japan), which can be inserted from the nose.
Compared with conventional gastroscopy, in which gastroscopes are inserted from the mouth, the major characteristic of this method is ‘not causing the vomiting reflex’.
According to some data, more than 9 patients out of 10 answered that it was easier for them to receive the examination with a gastroscope inserted from their nose.
The nasogastric endoscope we use is as thin as spaghetti, but it is usable for biopsies (collecting and examining tissue samples).
For those who feel uncomfortable receiving transnasal examination, we also use a gastroscope with the smallest diameter in Japan (as of February 2017) to be inserted from the mouth.
○Advantages of transnasal endoscopy
The advantages of transnasal gastroscopy compared with transoral methods are as follows:
- Rarely causing vomiting
Have you ever felt like vomiting, when you visited a hospital due to the common cold, and they held back your tongue with an instrument like a spatula? Some people experience this even during tooth-brushing. This is called the ‘gag reflex’.
The occasional occurrence of the gag reflex tends to make conventional transoral gastroscopy uncomfortable. In contrast, transnasal gastroscopy, in which a gastroscope is inserted without touching the root of the tongue, rarely causes such a reflex, preventing vomiting during the procedure.
- Allowing conversations with the practitioner during the procedure
With your mouth covered, you cannot converse during transoral gastroscopy. In the case of transnasal gastroscopy not involving the mouth, conversations are possible, consequently contributing to the safety of the examination.
- Allowing eating/drinking in 30-60 minutes
In conventional preparatory procedures, local anesthesia is performed extensively from the mouth to throat.
This leads to the necessity of refraining from drinking and eating for at least 2 hours after the examination.
As transnasal gastroscopy only requires a small amount of local anesthesia in the nasal cavity, you can drink and eat in about 1 hour after the completion of the examination.
- A repeat rate of 90%
In a questionnaire survey involving participants with experience of receiving both nasogastric and conventional endoscopies, more than 90% desired to receive the former again next time.
As nasogastric endoscopy reduces distress during and limitations after the procedure, most respondents regarded it as ‘far more comfortable than endoscopy involving the mouth’.

Compared with conventional transoral gastroscopy, transnasal gastroscopy is much more comfortable at least in the sense that it does not cause the gag reflex. In addition, in our facility, practitioners’ skills contribute not only to the feasibility of such a comfortableness, but to the highest-quality examination throughout the process of initially inserting a gastroscope from the nose and observing the gastric mucosa.
Explaining in detail, it is necessary for doctors who insert gastroscopes from the nose to acquire detailed knowledge of nasal anatomy, and master elaborate techniques for gastroscope insertion, which have not been needed by conventional digestive endoscopists. Devised methods and experience also markedly influence pre- and post-examination procedures, such as nasal anesthesia. Some hospitals finally choose oral endoscopy due to an excessively narrow nasal cavity, or emphasize the possible occurrence of persistent nasal bleeding or pain during gastroscope insertion, but this signifies that their examination skills are insufficient.
As a matter of fact, in our facility, transnasal gastroscope insertion has been infeasible due to an excessively narrow nasal cavity or for other reasons in only approximately 0.1% of all cases (about 1 in 1,000 patients, including those in whom the endoscope would have passed, if forced, but we did not). Nasal bleeding (slight bleeding as a result of rubbing the nasal mucosa during gastroscope insertion from the nose) also occurs in our facility, but it is just a small amount of blood observed when blowing the nose after the examination. Major bleeding is very rare. As for nasal pain during the insertion, there are naturally marked differences in skills and experience between hospitals performing 500 and 3,000 transnasal gastroscopies annually.
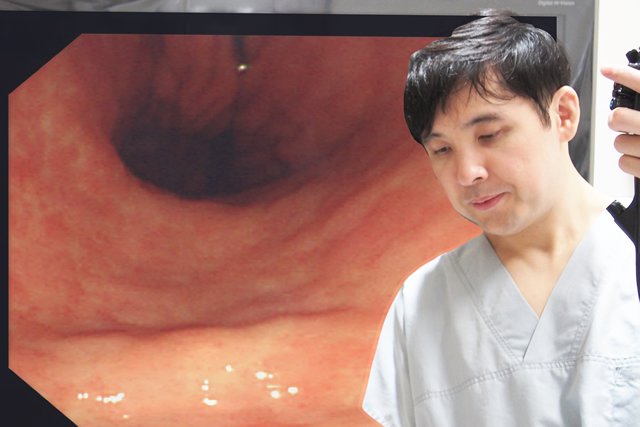
The image quality that had previously been a disadvantage of transnasal gastroscopy has also improved to a level similar to that in conventional transoral gastroscopy. As the slight dimness of the screen can be sufficiently made up for by practitioners’ proximity manipulation techniques and staining, the former’s observation capacity is currently similar or even higher than that of the latter under certain conditions.
Colonoscopy is a procedure to observe the entire large intestine and part of the small intestine, inserting a thin tube (about 1 cm in diameter) with a high-performance camera mounted at the tip from the anus.
It facilitates the accurate diagnosis of colon cancer that develops in more than 80,000 Japanese people annually (the second highest prevalence among all cancers, and the number of patients is steadily increasing), in addition to colon polyps and inflammatory bowel diseases causing fecal occult blood, abdominal pain, diarrhea, constipation, blood in stool, or other disorders.
Using colonoscopy, it is possible not only to identify colon cancer in the early stages, but also to prevent it by removing benign polyps.
LaLaport Yokohama Clinic performs painless colonoscopy.
○Colonoscopy-related distress markedly varies depending on practitioners’ skills.
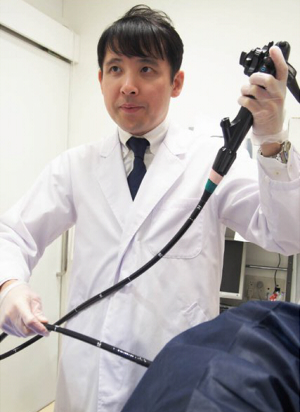
We perform ‘painless colonoscopy’; our practitioners’ highest-level skills make it possible to perform this procedure with almost no pain. Using an original, advanced technique developed by us to insert endoscopes completely airlessly and linearly into the deepest part of the large intestine, like magic it is possible to perform colonoscopy without abdominal tension or pain.
In order to master this technique, it is necessary to perform at least 5,000 colonoscopies. This is far greater than the 100 as a criterion for the Japan Gastroenterological Endoscopy Society to certify doctors specializing in this area. In addition to such experience, extensive expertise is also needed, suggesting that few domestic doctors are able to perform this technique.
To realize ‘painless’ colonoscopy, we also use an endoscope which is the softest (reducing the burden on the intestines) of all cutting-edge products of Olympus, which has the top market share in Japan, as well as mild sedatives. These mild sedatives (not anesthetics) enable patients to converse with the practitioner while observing images of the surface of their intestines during colonoscopy. This is completely different and more advanced than the ‘painless colonoscopy’ performed in other medical institutions using (whatever insertion method and) large amounts of painkillers to complete the procedure while patients are ‘sleeping (unaware of pain)’.
When the director of our facility belonged to the University of Tokyo Hospital, he performed the largest number of colonoscopies in the Department of Colon and Rectal Surgery. He was also evaluated by patients the most favorably ever in private facilities specializing in endoscopy. While supervising junior doctors in university hospitals, he also devotes himself to the dissemination of his original examination methods among endoscopists through the Internet and his writings. As of 2015, the total number of colonoscopies performed in our facility exceeds even those in all university hospitals.
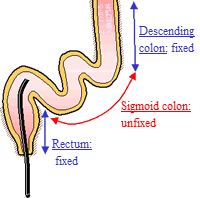
The rectum (located nearest the anus) and descending colon are fixed on the periphery, while the sigmoid colon is unfixed, dangling, and in an unstable state. Distress related to colonoscope insertion varies depending on whether the sigmoid colon is stretched or not.
In conventional colonoscopy, colonoscopes are pushed from the anus (‘push method’). For example, supposing that you are putting on a shirt, the sleeve is the large intestine, and your arm is an endoscope. Similarly to your arm hitting the shirt when it passes through the sleeve, the S-shaped colon is stretched with the insertion of the endoscope. The sections corresponding to your fist and elbow hit the internal wall of the large intestine. This is why patients commonly experience ‘abdominal tension and pain’ during colonoscopy.
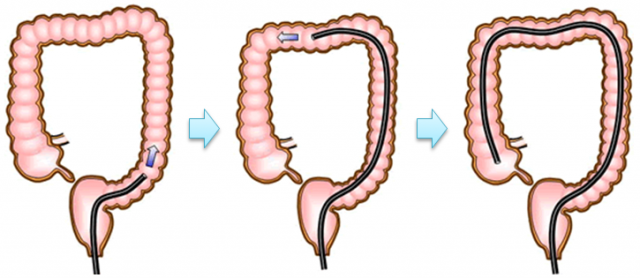
At LaLaport Yokohama Clinic, colonoscopy is performed using the ‘pull method’ (please see the figure below), rather than the push method. The pull method enables us to insert colonoscopes linearly, and minimize the burden on the large intestine.
Furthermore, by avoiding stretching the large intestine, it is possible to reduce distress due to abdominal tension, as well as the risk of accidents/incidents. It is regarded as very difficult to master this method, as it is only usable for master-class doctors with extensive experience of performing colonoscopy.
○Push method (conventional colonoscope insertion method)
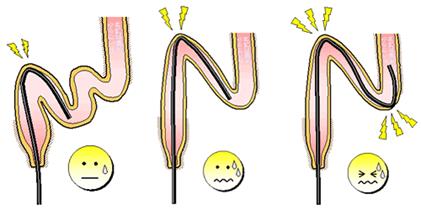
Currently, colonoscopy is being performed using the push method in most hospitals.
In this method, the procedure proceeds with a colonoscope being pushed into the intestines. If this is performed by doctors with standard skills, the sigmoid colon stretches out, and becomes tense, possibly causing abdominal bloating or pain.
In medical institutions that only perform colonoscopy using this method, large amounts of strong sedatives are needed to prevent pain during the procedure.
○Merits of the pull method (painless colonoscope insertion method)
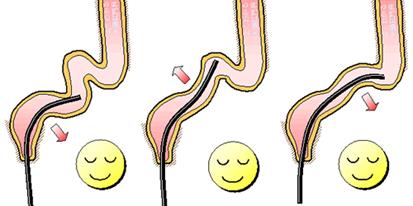
The intestines are carefully folded like an accordion to insert an endoscope ‘linearly’ until it reaches the descending colon. Requiring a careful operation to avoid stressing the intestines, this takes a longer time than the push method, but it realizes a painless procedure.
The pull method attaches importance to enabling patients to receive colonoscopy comfortably (or without pain) by reducing their burden.
○Further advanced colonoscopy using a ‘completely airless and linear colonosope insertion method’
In the conventional pull method, air is injected to observe the inside of the intestines. There is a more patient-friendly method, which is completely airless: ‘completely airless and linear colonosope insertion method’. Only doctors beyond the ‘master class’ are able to use this. Director Ohnishi at LaLaport Yokohama Clinic performs colonoscopy using this method.

